The most common indication for the removal of third molars is pericoronitis, non-restorable caries or internal resorption. Yet, when a third molar is close to the inferior alveolar nerve, the risk of nerve injury is high. So the practitioner is put in a tough spot, having to accept the high risk of eventual parasthesia or neuropathic pain, with no other clear alternative treatment options.
Coronectomy of a tooth has long been contraindicated in the theoretical world, with no clinical evidence. A fundamental principle of coronectomy is that the retained root fragment remains vital, with a non-inflamed pulp and healthy surrounding periodontium. In the theoretical world, it has been said that any degree of pathology, including incipient decays, can inherently inflame the tooth pulp, and therefore the tooth is not eligible to receive coronectomy. This creates a blanket rule for the procedure in general.
Shokouhi et al. has shown that coronectomy roots retain vitality; counteracting the previous understanding that vitality is lost when the coronal portion of the tooth is removed. This has also been shown even when the coronal tooth has decay or internal resorption, which would be subsequently removed during coronectomy.
With careful case selection with various imaging techniques, we can now ensure that a tooth has a vital pulp and sound surrounding periodontium. 3D assessment of the tooth can provide the depth of the pathology in multiple planes, and its proximity to pulp horns. Radiographic evidence of apical disease or suspected pulp infiltration of pathology would contraindicate this procedure. Furthermore, in many cases, the decision to keep the root intact should be made intraoperative, with direct view of the pulp following coronectomy.
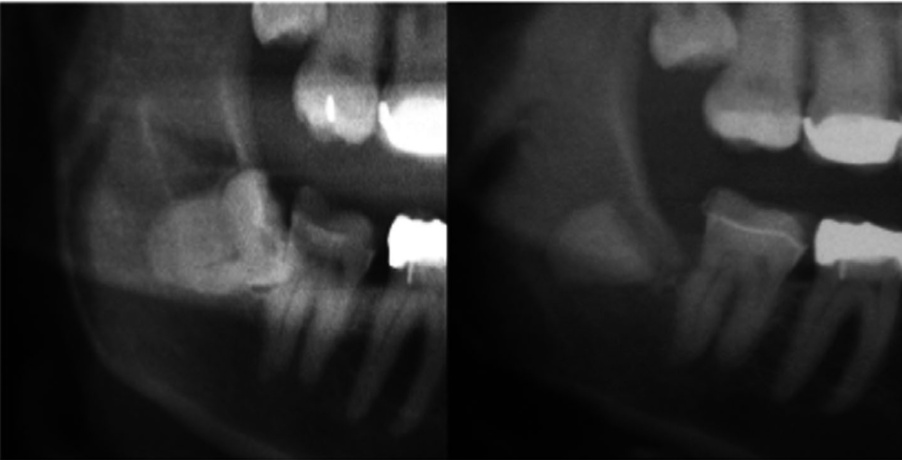
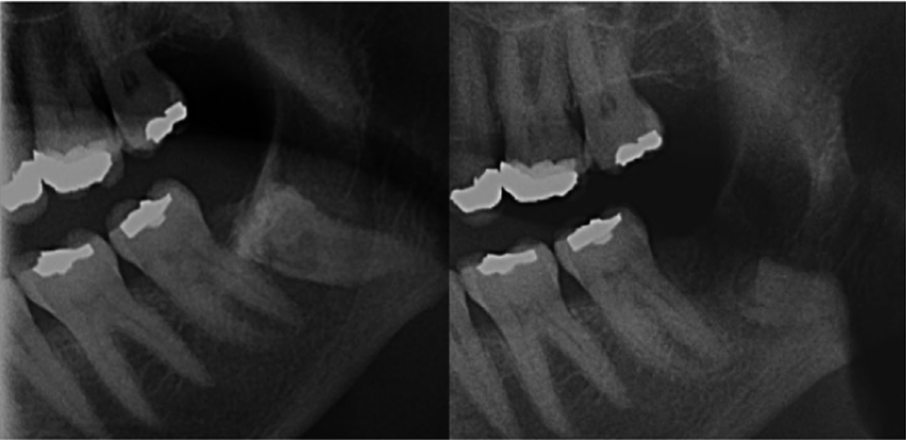
A 2019 study followed 20 patients that underwent coronectomy for mandibular third molars that were dangerously close to the inferior alveolar nerve. The average age of the patients were 35 years old, ranging from 18 to 73 years. The teeth involved in the study all had active pathologies including caries (enamel and dentinal) and internal resorption. All had no evidence of pulp pathology.
Following the surgery, all patient were monitored at 1 month and 12 month appointments. During the 1-month follow-up 9% showed post-op complications consisting of alveolar osteitis and surgical site infection, which were treated with antibiotics. The complications were not associated with any root infections, indicating that the infections were related to the surgical site, rather than an odontogenic infection. No further complications were seen at 12 months for any patient. During this time all patients were asymptomatic and did not require root retrieval.
Coronectomy can be a viable treatment option for mandibular third molars when they are an obvious danger to nerve injury.


