There are only a few things that can make a dentist’s heart skip a beat. Perforations are one of them. Furcation perforations can cause your heart to skip two beats, and want to cancel the rest of the day.
Fortunately, thanks to ongoing research on the possibilities of bioactive materials – such as mineral trioxide aggregate (MTA), your regular cardiac rhythms can be restored.
When faced with a perforation, the prognosis of the tooth is dictated by a) the size and location of the perforation, b) the time elapsed from initial damage, and c) the possibility to clean and seal the area of the perforation. Luckily, it has been shown that we can achieve up to 80.9% success rate in the repair of root perforations, in a non-surgical approach using MTA.
Clinical Presentation – by Angerame et al.
A 26-year-old male presents (referred by a colleague) due to a lower right first molar furcal perforation, occurring during a cavity restoration. Pre-operative reports and radiographs show that the pulp was asymptomatic, free of pathology, and that the decay did not involve the pulp.
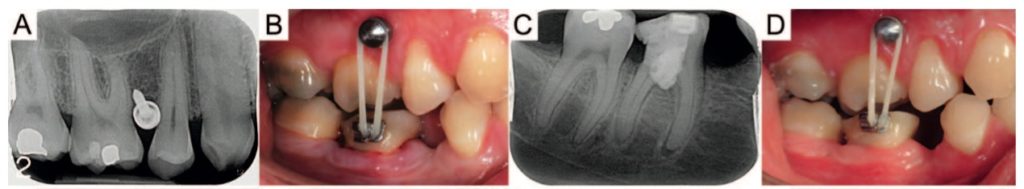
During cavity preparation, the pulp was exposed, endodontic treatment was initiated, and in an attempt to locate the canal orifices – root furcation perforation occurred (Figure 1).
Treatment Rendered

The following is the approach taken to maintain pulp vitality and restore the tooth, through a multidisciplinary approach.
- Rubber dam placed, temporary filling removed, and canal orifices located under microscope magnification.
- As the canal orifices and periodontium was not seen to be bleeding, pulp capping and perforation repair with MTA was done. Initially, the endodontic access was disinfected with 2.5% sodium hypochlorite solution for 10 minutes. MTA cement was placed into the defect. In order to achieve coronal seal, a hard-set calcium hydroxide base was applied.
- The coronal access of the tooth was restored with composite resin, following enamel and dentin etching (37% phosphoric acid) and boding with All-Bond 3 system (Bisco).
- Weekly follow up appointments were done for one month reporting no pain or dysfunction by the patient.
- Predicting the final crown restoration needed for this tooth, orthodontic extrusion and biological width realignment were considered. Tooth extrusion was chosen as an alternative to crown lengthening, as it would retain sounds tooth structure, and prevent marginal bone loss following final restoration.
- Orthodontic extrusion protocol included (Figure 2):
- Local anesthesia administration.
- Mini-screw placement between first molar and first premolar in the opposing jaw.
- Bonding of orthodontic tube with hook on the buccal surface of the lower right first molar.
- Rubber band was connected from the head of the screw placed in the first quadrant to the buccal tube on lower right first molar.
- Following 2 months of orthodontic extrusion, crown lengthening was done.
- Local anesthesia was administered.
- Distal papilla was incised and displaced, combined with 3 mm releasing incision on the mesial of the lower right first molar.
- Interproximal bone crest was remodeled with diamond burs – only what was needed to restore the biological width from the future restoration margins.
- A bonded splint was applied between the lower right first molar and lower right second molar, to stabilize the position following orthodontic extrusion – the splint kept for two weeks.
- Crown preparation
- Circumferential crown preparation was done with feather-edge margins.
- A temporary acrylic crown was placed – aiding in soft tissue conditioning and orthodontic stabilization (due to occlusal contacts).
- The permanent crown was manufactured with composite resin and cemented using RelyX Unicem self-adhesive resin cement.
Annual post-op/ monitoring appointments were kept for eight years – showing no complications.


